Key Messages from the CIHR Mid-Term Knowledge Mobilization Virtual Event: Addressing Infectious and Congenital Syphilis in Canada
Background
Since 2017, there has been a dramatic increase in rates of infectious syphilis, with rates reaching 36.1 per 100,000 by 2022Footnote 1. Since then, there has also been a major shift in the demographics of the populations affected. Although gay, bisexual and other men who have sex with men (gbMSM) continue to have the highest rates of syphilis nationwide, rates of infectious syphilis increased by 256% among women compared to 68% among men between 2018-2022. During this period, reported rates of infectious syphilis among females aged 15 to 39 years increased annually and the 2022 national reported rate was 239% higher than the 2018 rateFootnote 1. As a result of these changing demographics, a concurrent re-emergence of congenital syphilis has occurred with cases increasing from 17 in 2018 to 117 in 2022 – a 599% increaseFootnote 1.
Early diagnosis of infectious syphilis, followed by appropriate treatment, is critical to reducing transmission for both infectious and congenital syphilis. In Canada, universal syphilis testing is considered part of standard prenatal care. Unfortunately, because of stigma, racism, sexism and other forms of systemic and structural discrimination, access to sexually transmitted and blood-borne infections (STBBI) testing and prenatal care is particularly limited for people from Indigenous and rural, remote and isolated communities, as well as for people who use drugs or experience homelessness. There is an urgent need to improve access to syphilis testing and prenatal care for these communities.
In September 2023, the CIHR HIV/AIDS and STBBI Research Initiative, in partnership with the Centre for Research on Pandemic Preparedness and Health Emergencies (CRPPHE), the Institute of Indigenous Peoples' Health (IIPH), the Public Health Agency of Canada, and Indigenous Services Canada launched the Operating Grant: Addressing Infectious and Congenital Syphilis in Canada funding opportunity to respond to the growing syphilis crisis in Canada by supporting implementation science and intervention research. Over $2.6M was invested to support seven teams to advance research and knowledge mobilization in two research areas: implementation science for syphilis point-of-care testing (POCT), and new models of care for prevention of congenital syphilis.
Event description
On December 12th, 2024, CIHR, in partnership with the Public Health Agency of Canada and Indigenous Services Canada, hosted a virtual knowledge mobilization event to support the funded research teams in sharing their early successes, insights and key challenges with each other and with decision makers, knowledge users and the funders. Research teams were asked to provide input on the objectives, format and focus of the event, and to invite knowledge users and decision makers who would benefit from learning more about their work. The objectives of the event were to facilitate knowledge sharing across the research teams and with government officials, public health professionals and community partners, and to identify opportunities and discuss barriers related to their research projects.
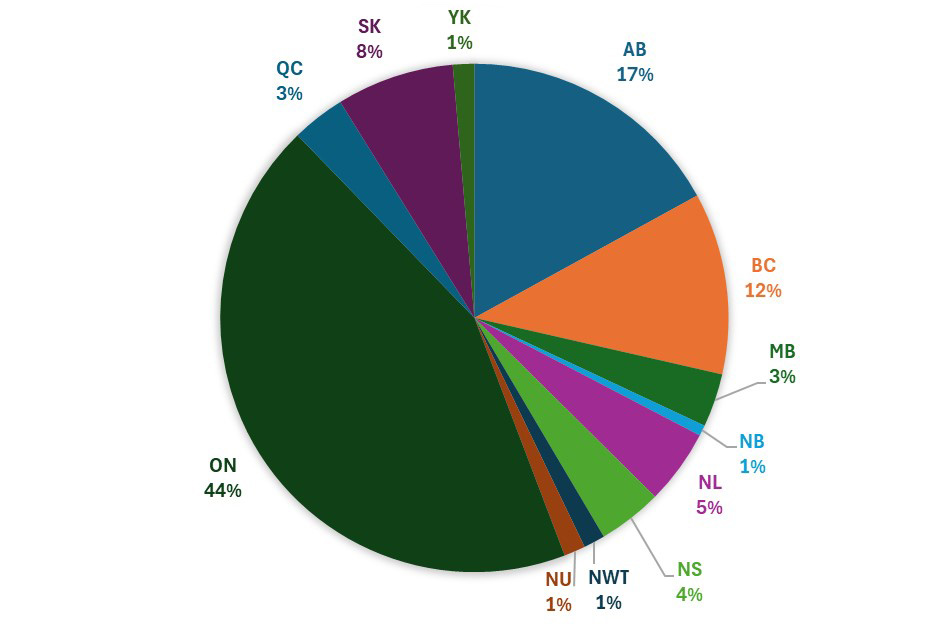
Excluding speakers and organizing staff, just under 150 participants attended the event. Of those, approximately 50% of the participants were from federal/public/provincial health agencies, 25% were from community organizations, and 23% were from academic institutions. The geographical representation of the participants is as follows:
Long description
Geographical Distribution of Participants
- Ontario: 44%
- Quebec: 3%
- Saskatchewan: 8%
- Yukon: 1%
- Alberta: 17%
- British Columbia: 12%
- Manitoba: 3%
- New Brunswick: 1%
- Newfoundland and Labrador: 5%
- Nova Scotia: 4%
- Northwest Territories: 1%
- Nunavut: 1%
The meeting was chaired by Dr. Charu Kaushic, Scientific Director of the CIHR Institute of Infection and Immunity. The event was opened by Grandmother Irene Compton, who provided a welcome and prayer, followed by frontline health professionals Noel Ives and Nikki Williamson, who provided insights on the impact of infectious and congenital syphilis on the communities and colleagues they work with. The research teams' nominated principal investigator, or a delegate, presented an overview of their early successes and key challenges, followed by an opportunity for discussion with each other and with participants. Projects presented were as follows:
- Rapid point-of-care syphilis testing in an urban community-based prenatal care program for populations with barriers to healthcare access: A prospective implementation study examining acceptability, feasibility, and effectiveness for timely diagnosis and treatment of syphilis in pregnancy
Laura Erdman, McMaster University - wahkohtowin (Kinship beyond the immediate family) Community-based models of care to reach and support Indigenous and racialized women of reproductive age and pregnant women in Canada for the prevention of congenital syphilis
Margaret Kisikaw Piyesis, Communities, Alliances & Networks - Towards the eradication of congenital syphilis in Canada
Deborah Money, University of British Columbia - Dual syphilis and HIV: evaluation of POC and self-test by untrained persons, peers and intended users
Sean Rourke, Unity Health Toronto - Breaking barriers: expanding syphilis point-of-care testing and immediate treatment to meet the needs of underserved communities
Sahar Saeed, Queen's University - Scaling up point of care testing and linkages to care for syphilis and HIV in rural, remote, and Indigenous populations in central Alberta
Ameeta Singh, University of Alberta (presented by Alexa Thompson) - Stopping syphilis transmission in Arctic communities through rapid diagnostic testing in non-traditional testing sites (STAR-NT study)
Cedric Yansouni, Research Institute of the McGill University Health Centre
The event also included breakout sessions with panels of researchers discussing community engagement and knowledge mobilization in underserved communitiesFootnote i related to syphilis POCT testing and prevention of congenital syphilis in perinatal care settings, as well as a panel discussion focused on overcoming barriers to research and knowledge mobilizationFootnote ii. Participants, including knowledge users, were invited to reflect on what they heard and learned, and the meeting was closed in a good way by Grandmother Irene. A second virtual knowledge mobilization meeting will be organized in 2025/26 to share additional insights and research findings resulting from these projects.
Key themes and messages
Data collection, race-based data and real-time access to data
- Numerous research team members, speakers and participants reinforced the critical need for consistent data collection across all jurisdictions. Inconsistent interpretation of privacy and data sharing laws and guidance from authorities, and limited access to surveillance data, including race-based data, is impeding the effective delivery of interventions and the overall response to this crisis.
- The importance of Indigenous data sovereignty and governance in data sharing was emphasized consistently.
- A commitment from all partners is required to establish and support the requirements, guidelines and processes necessary for a syphilis elimination strategy, and to address the systemic and structural racism that continues to delay progress on this issue. Speakers pointed to the COVID-19 pandemic as evidence of how quickly data can be collected and shared; it is possible if leadership is on board.
- Improved integration of POCT results into surveillance systems would enhance real-time understanding and support better linkage to care.
- Sharing data in accessible formats for communities, providers and decision makers can support more informed and timely responses.
Upholding Indigenous rights and ways of knowing
- The rights, priorities and needs of First Nation, Inuit and Métis communities must be advanced and respected by research and research processes. Indigenous communities are most informed about their needs and how to advance research that addresses their priorities.
- Indigenous communities approach research questions from a holistic understanding of the issue and recognition of the interconnection of health and community well-being.
- Indigenous ways of knowing must be centered and respected. A respectful and distinctions-based approach to health and wellness, tailored to the unique interests, priorities and circumstances of the Indigenous Peoples, was emphasized.
- Culturally grounded approaches such as ceremony, land-based practices, and arts-based knowledge sharing can strengthen engagement and support healing and empowerment.
- Supporting Indigenous-led care, including peer and community-led initiatives, enhances the cultural safety and effectiveness of interventions.
Community leadership and trusting relationships
- Building and maintaining trust with and within communities is critical to successful interventions. The level of community leadership and ownership of an intervention strongly impacts the potential for success, ex. encouraging testing, collecting data.
- Community leadership facilitates engagement, recruitment and retention.
- Providing services in trusted spaces and engaging peers or community health representatives can improve uptake and foster stronger relationships.
- Embedding services within existing local wellness initiatives, and respecting the pace and priorities of communities, supports more sustainable outcomes.
Knowledge mobilization
- Approaches to community knowledge mobilization should not be pre-conceived, but rather co-developed with communities. This requires early engagement at the proposal development to avoid tensions arising from perceptions of imposing pre-established plans.
- Communities often contribute to research data, but don’t see the benefits or impact of its use.
- The importance of providing data and research outcomes to those who can implement changes and real-time solutions was discussed.
Role of public health systems
- Public health departments vary considerably, for many reasons, in their access to and uptake of new technologies such as POCT.
- Participants highlighted the lack of equity in healthcare systems; the need for accessible and affordable healthcare for all, along with the disconnect between the healthcare services availability and the ability to connect individuals to care.
- The importance of community-led initiatives in improving healthcare access and outcomes was emphasized.
- Some participants advocated for innovating within existing systems, while others highlighted the inherent racism and inequity of current systems.
- Embedding POCT within broader care pathways, rather than using it as a stand-alone tool, helps to ensure appropriate follow-up and treatment.
- Supporting task-shifting strategies, such as training peers and community members to provide testing, education, and linkage to care, can help address workforce gaps and build local capacity.
- Sustainable care in rural, remote, and urban settings requires long-term investment and flexible funding models that are responsive to local needs and not siloed by program or disease area.
Next steps
A second virtual knowledge mobilization event is anticipated to take place in the winter 2026 for continued knowledge sharing among research teams, decision-makers and knowledge users to inform future work or policy directions.
For more information
For additional information, please contact the HIV/AIDS and STBBI Research Initiative at HIVAIDS-VIHSIDA@cihr-irsc.gc.ca or support-soutien@cihr-irsc.gc.ca.
Canada's research response to HIV/AIDS and STBBI is propelled by the CIHR HIV/AIDS and STBBI Research Initiative. With strategic and scientific leadership from the CIHR Institute of Infection and Immunity, the Research Initiative invests approximately $21 million per year to support researchers and trainees through research funding aligned with priorities identified in the 2022-2027 CIHR HIV/AIDS and STBBI Strategic Plan. These priorities advance the actions identified in the Pan-Canadian STBBI Framework (Reducing the Health Impact of Sexually Transmitted and Blood-Borne Infections in Canada by 2030: A Pan-Canadian STBBI Framework for Action) and Canada's Action Plan on STBBI (Government of Canada's sexually transmitted and blood-borne infections (STBBI) action plan 2024-2030). The CIHR HIV/AIDS and STBBI Research Initiative is guided by the CIHR HIV/AIDS and STBBI Research Advisory Committee (CHASRAC), which is comprised of members from diverse areas of expertise, and includes academic researchers from a range of disciplines, people with lived/living experience, and representatives from community organizations.
- Date modified: